Clinical Practice
Incidence of Orthostatic Hypotension During Mobilization Following a Total Joint Arthroplasty
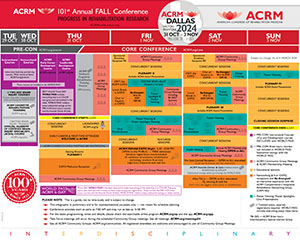
Saturday, November 2, 2024
10:15 AM - 10:30 AM
Location: Station 4: ROOM: POSTERLAND / Trinity Poster / Exhibit Hall REGION: Tower Lobby Level >>>

Haily Roth, PT, DPT
Physical Therapist
Lehigh Valley Health Network
Allentown, Pennsylvania, United States
Stephanie Hack, PT, DPT
Physical Therapist
Lehigh Valley Health Network
Allentown, Pennsylvania, United States
Presenting Author(s)
Non-presenting author(s)
Research Objectives: To investigate the incidence of orthostatic hypotension
Design: Process Improvement Study assessing vitals during mobilization with physical therapy and nursing staff as indicated
Setting: Lehigh Valley Health Network-Tilghman Hospital
Participants: 188 records of THA and TKA patients
Interventions: Nursing and physical therapy assessed vitals, symptoms and ability to be out of bed and tolerate being out of bed were monitored until the patient was able to successfully remain out of bed after surgery
Main Outcome Measures: The primary outcome was to identify the incidence of orthostatic hypotension post-TJA.
Results: Of 170 patients that had received a THA/TKA at LVHN-TH, we collected 188 records. We compared overall data to TKA/THAs, surgeons, anesthesiologists, CRNAs, type of anesthesia, if the PT evaluation was completed POD #0, if the patient was able to mobilize POD #0, if the patient could ambulate/transfer to a bedside chair, the patients OOB tolerance time, length of stay, age and amount of IV fluid received in the OR.
Overall, 52/188 records (27.66%) had +OH with 16 of those being symptomatic (8.51%). 29/188 (15.43%) of records had symptoms of OH with mobilization, no matter their vital sign response.
In regards to being able to get out of bed and transfer/ambulate to a bedside chair, 154/188 (81.91%) of records were able to transfer/ambulate to bedside chair. 41/154 (26.62%) of those records had +OH and 8/154 (5.19%) had symptoms to the +OH. 17/154 (11.04%) of records had symptoms, no matter their vital sign response. 34/188 (18.09%) of records were not able to transfer/ambulate to bedside chair.
Conclusions: Our study shows that there is a high level of +OH (27.66%) following joint replacement. There are differences in the number of records of +OH and if the patient is symptomatic depending on surgeon, anesthesiologist, CRNA and type of anesthesia. Individuals with +OH and symptoms did receive slightly less fluids on average than the overall average fluid given to a patient undergoing a total joint replacement. Individuals with positive symptoms of OH spent less time out of bed with initial mobilization compared to the average time spent out of bed. Our study shows a positive correlation between length of stay and +OH and symptoms associated with OH.
Author(s) Disclosures: N/A
Design: Process Improvement Study assessing vitals during mobilization with physical therapy and nursing staff as indicated
Setting: Lehigh Valley Health Network-Tilghman Hospital
Participants: 188 records of THA and TKA patients
Interventions: Nursing and physical therapy assessed vitals, symptoms and ability to be out of bed and tolerate being out of bed were monitored until the patient was able to successfully remain out of bed after surgery
Main Outcome Measures: The primary outcome was to identify the incidence of orthostatic hypotension post-TJA.
Results: Of 170 patients that had received a THA/TKA at LVHN-TH, we collected 188 records. We compared overall data to TKA/THAs, surgeons, anesthesiologists, CRNAs, type of anesthesia, if the PT evaluation was completed POD #0, if the patient was able to mobilize POD #0, if the patient could ambulate/transfer to a bedside chair, the patients OOB tolerance time, length of stay, age and amount of IV fluid received in the OR.
Overall, 52/188 records (27.66%) had +OH with 16 of those being symptomatic (8.51%). 29/188 (15.43%) of records had symptoms of OH with mobilization, no matter their vital sign response.
In regards to being able to get out of bed and transfer/ambulate to a bedside chair, 154/188 (81.91%) of records were able to transfer/ambulate to bedside chair. 41/154 (26.62%) of those records had +OH and 8/154 (5.19%) had symptoms to the +OH. 17/154 (11.04%) of records had symptoms, no matter their vital sign response. 34/188 (18.09%) of records were not able to transfer/ambulate to bedside chair.
Conclusions: Our study shows that there is a high level of +OH (27.66%) following joint replacement. There are differences in the number of records of +OH and if the patient is symptomatic depending on surgeon, anesthesiologist, CRNA and type of anesthesia. Individuals with +OH and symptoms did receive slightly less fluids on average than the overall average fluid given to a patient undergoing a total joint replacement. Individuals with positive symptoms of OH spent less time out of bed with initial mobilization compared to the average time spent out of bed. Our study shows a positive correlation between length of stay and +OH and symptoms associated with OH.
Author(s) Disclosures: N/A
Learning Objectives:
- Upon completion, participant will be able to understand incidence of orthostatic hypotension post joint replacement in acute care orthopedics.
- Upon completion, participant will be able to understand if orthostatic hypotension post joint replacement has an impact on the ability to be out of bed.
- Upon completion, participant will be able to understand if orthostatic hypotension post joint replacement has an impact on out of bed tolerance.

.jpg)
.jpg)
.jpg)